Menu
Table of Contents
Bipolar
Table of Contents
Related Subjects
You have questions about bipolar disorder. Maybe many, many questions: What causes it? What treatments are best? We’re going to answer them as clearly and thoughtfully as possible, with help from the top doctors around. Our hope is that you’ll find some peace right now—and plenty of solutions moving forward.
What Is Bipolar Disorder?
Like the name suggests, bipolar disorder is marked by polar opposite mood swings—at one point, you feel like you can conquer anything; at another, you can barely get your butt out of bed. Once called manic depression, bipolar disorder affects up to 5.7 million adults. It impacts both men and women equally and the typical onset of symptoms usually occurs between ages 15-25. Of course, those years are notoriously emotional ones—first loves, college, new careers! Throw wonky energy levels into the mix, and, oof, things just got more complicated. After all, how hard is it to plan your schedule or navigate your life when you don’t know which “you” you’re getting that week?
Like many mental disorders, bipolar illness is genetic and tends to run in families, meaning oftentimes, one or more family members also have a form of bipolar disorder. (It’s important to note that the illness can start in early childhood or as late as the 40s-50s.)
Are There Different Types of Bipolar?
Yes, there are four types, each defined by their own symptoms and episodes. Three of the most common include Bipolar I disorder, Bipolar II disorder, and cyclothymic disorder. Here’s what you need to know.
Bipolar 1 Disorder
Bipolar I is characterized by the occurrence of at least one manic episode, preceded or followed by a hypomanic or major depressive bout lasting at least a week. Manic episodes may be so severe they significantly disrupt your daily functioning or may even trigger a break from reality (psychosis). People who have a manic episode often describe it as feeling invincible and euphoric. You’ll usually experience three or more symptoms such as inflated self-esteem, decreased sleep, being more talkative, distracted, goal-directed, or idea-driven, or get involved in activities that can have painful or even financial consequences, like spending thousands (you don’t have) on a designer handbag—or five. You may even need hospitalization with bipolar I. The disorder is characterized by the distinct periods of mania and depression.
Bipolar 2 Disorder
If you are living with Bipolar II, you’ll likely experience at least one major depressive episode lasting two weeks or more and at least one hypomanic episode lasting at least four days. But you won’t have manic episodes, says Anandhi Narasimhan, MD, a double board-certified child, adolescent, and adult staff psychiatrist at Masada Homes in Gardena, California, with a private practice in Westwood. With bipolar II, episodes of mania are replaced with hypomania, a less severe form of mania, but one that can still impact your daily life. Bipolar II symptoms don’t typically require hospitalization. However, the symptoms may be harder to identify with this type because they’re less severe, prolonging diagnosis and treatment.
Cyclothymic Disorder
Cyclothymic disorder is a rarer form of bipolar affecting about 3.29 million people in the U.S. that’s characterized by at least two years of multiple occurrences of hypomania and depressive symptoms. While symptoms are less severe than typical hypomanic episodes and major depressive episodes, they are more chronic. Symptoms can stay constant for at least two months. People who have cyclothymia are affected by impulsivity and poor decision making, affecting relationships, family, and social life, and they may also experience problems with the law and financial difficulties. Less than half of those with cyclothymia will go on to develop a more severe form of bipolar disorder.
What Are the Signs and Symptoms of Bipolar Disorder?
Before you self-diagnose, remember, we’re not talking about being down in the dumps over a breakup or having a bad day, or being super-happy over a promotion or a new relationship. These are natural highs and lows that everyone experiences. The classic symptoms of bipolar disorder are kind of like being on the steepest roller coaster, where moods dip from the lowest depression to the highest high (mania or hypomania).
Manic Episodes
When you live with bipolar disorder you can feel energetically happy with boundless energy during manic states. You may make reckless decisions or act impulsively. You can get irritated and agitated easily and act out, you can even feel euphoric, have a decreased need to sleep or insomnia, and have racing thoughts or a grandiose self-image.
You may feel elated, like you just won the lottery, while really, it’s just any old day and you’re slogging through a pile of dirty dishes. Hypomania, which people with bipolar may also experience, is a less severe form of mania, where you generally feel pretty good–with a better sense of well-being and higher productivity.
There’s a laundry list of different symptoms for this manic phase, and they generally centre around an elevated or irritable mood. They may include goal-directed activities like staying up all night cleaning obsessively or going on a shopping spree—things you wouldn’t do typically. Manic behaviours may interfere with school, work, and relationships. Specific signs and symptoms include:
- Abnormally upbeat. This isn’t just a normal good mood. We’re talking feeling zippy and energized, even in situations that don’t warrant it, like feeling giddy taking out the trash. It’s like you’re not in charge of your mood, responding to your environment. Instead, you’re just stuck on cheerful mode.
- Euphoric. This is beyond happy; your excitement and energy are almost uncontained.
- Jumpy. You can imagine when you have this kind of energy surge, you feel reactive. Picture electricity zooming through your body.
- Racing thoughts. It’s hard to keep track of everything swirling around in your brain—you have all kinds of ideas, plans, and opinions.
- Abnormally talkative. You want to express all of these thoughts, so you’re extra chatty and may jump from topic to topic.
- Pressured speech. This is a giveaway sign of a manic episode. It goes along with being talkative and is marked by a stream of talking, without pausing in the normal way you would during a conversation. It’s like just bulldozing right through and not allowing the other person to talk, talking over them.
- Wired. People having manic episodes feel like they can stay up all night or don’t need as much sleep.
- Excess energy. You have all these ideas and energy and start taking on a lot of new projects.
- Poor decision-making. As you might imagine, a manic episode is not a great time for decision-making. Your emotions are skewed, and your sense of consequence and danger are dulled. It’s a pretty scary combo. You may take risks like making financial investments, engaging in sexual indiscretions, or going on shopping sprees.
- Easily distracted. With all this internal racing going on, it’s nearly impossible to focus.
- Cranky and/or impatient. You feel like no one can keep up with you, and it’s frustrating.
- Invincibility. Along with this surge of energy and risk-taking, you get a huge boost in self-confidence. Even people who are shy or humble may suddenly seem arrogant and think they can literally do anything.
- High sex drive. You’re constantly thinking about and wanting sex.
- Unattainable plans. You’re determined to book a trip to Paris—even though you don’t have the funds.
- Psychosis. A detachment from reality that may include delusions or hallucinations.
Depressive Episodes
And here comes the crash. You may feel overwhelming sadness or an urge to cry, experience feelings of hopelessness and worthlessness, and have a negative outlook on life. You may have an increased need to sleep, not be able to complete daily tasks and feel deeply demoralized. This isn’t just mild sadness but for some can be debilitating depression that can even lead to suicidal thoughts. Again, this can happen when nothing in your environment has brought on this mood.
“In the most severe instances of bipolar, psychotic features including hallucinations or delusions can be present during extreme mood events,” says Michael Pipich, MS, LMFT, a psychotherapist and author of Owning Bipolar: How Patients and Families Can Take Control of Bipolar Disorder.
Specific signs and symptoms include:
- Low energy. This is the kind of energy drain that makes you just want to lay on the couch or under the covers all day.
- Low motivation. You just don’t feel like doing anything.
- Loss of interest and finding no pleasure or interest in day-to-day activities. This is a classic depression syndrome—things that used to be interesting and fun hold no appeal anymore.
- Feeling sad, tearful, hopeless, or empty on a daily basis. Picture feeling blah with a tinge of sorrow, like the way you feel at the end of a really sad movie when you’re done crying, the credits are rolling, but you just can’t turn the tv off; it’s like you’re immobile.
- Hopelessness. You can’t picture anything good in the future.
- Weight fluctuations. Depending on whether depression zaps or increases your appetite, a person suffering may gain or lose a significant amount of weight.
- Feelings of fatigue. You feel so tired and just want to sleep. (Though insomnia is also a symptom.)
- Indecisiveness. Maybe it’s because you feel hopeless or ambivalent about everything, but you really can’t make your mind up, even about small things.
- Inability to concentrate. You lose your focus.
And just when you think your mood has hit rock bottom, the ride takes you back up to the summit with feelings of euphoria and endless energy. It’s these extreme mood swings that define bipolar disorder. They can occur as frequently as weekly, or, show up more sporadically—maybe just twice a year.
Unlike a predictable monthly cycle or known allergy that triggers a reaction, there’s no defined pattern or predictability to the mood swings—i.e. you can’t plan a job interview or vacation a week from Monday when you’ll be symptom-free. The condition just doesn’t work like that. And, there’s no rhyme or rhythm to which will come first, the depression or the mania or vice versa. What’s more, the length of time you’re in one state or the other can vary, too.
What Causes Bipolar Disorder?
Like most mental illnesses, researchers haven’t pinpointed a single cause, but it seems that a combination of genes and environmental factors can awaken bipolar. Scientists have learned that a number of genes are associated with the disorder, meaning it’s about 80 percent genetic. If you have a first-degree relative with the disorder, you’re at higher risk for developing it, and if you have relatives with other mental health conditions, you may have increased risk as well. But not everyone who has bipolar disorder in their family will get the illness.
Scientists have learned that a number of genes are associated with the disorder, meaning it’s about 80% genetic. If you have a first-degree relative with the disorder, you’re at higher risk for developing it, and if you have relatives with other mental health conditions, you may have increased risk as well. But not everyone who has bipolar disorder in their family will get the illness.
Environmental factors also play a role in developing bipolar. And these interact with genetic predispositions to trigger the onset of the disorder. These include diet, sleep, substance use and abuse, the stability of your relationships, the atmosphere in the home if you’re an adolescent, stress, and early childhood trauma. This means is that if you’re living with bipolar disorder, it was probably a mixture of genes and environmental factors or life events that triggered the disorder to present itself.
While some people who have bipolar have suffered from some type of early traumatic event, abuse, or a troubling and/or stressful episode, many others cannot link to anything specific in their past.
With those differences, it’s not surprising that bipolar disorder is frequently misidentified and mistreated. “Research shows that nearly two-thirds of people with bipolar have been misdiagnosed at least one time in their lives and will have suffered nearly 10 years of untreated symptoms before receiving proper care,” Pipich says.
This gap in treatment is usually the result of misunderstanding bipolar illness—how it presents itself in episodes that can come and go, and the stigma of having a chronic mental illness, especially when symptoms are present in a young person, explains Pipich.
And sometimes, other issues are simply masking the bipolar. Many patients will be diagnosed with the condition only after they seek sobriety for alcohol or drug abuse. Why the link? People often like how they feel when they are manic and think that level of creativity, productivity, and euphoria is helpful to their life so they try to replace it with substances like drugs and alcohol, explains Michelle English, LCSW, co-founder and clinical director of Healthy Life Recovery, a San Diego-based rehab and addiction center. “On the flipside, manic people with bipolar disorders may use substances to help them relax, sleep, and calm down,” English says.
What’s important is if you suspect you may have bipolar disorder, see your doctor so you can manage the condition and live a productive life without the ups and downs of extreme mood swings.
What’s Going On In The Brain?
Up until recently, researchers hadn’t been able to distinguish a person with bipolar’s brain from a person without the disorder on a scan. But science is making some tracks. A 2019 study that looked at the brains of people with bipolar and those with depression on functional MRI scans correctly differentiated their brains about 80% of the time.
The findings suggest differences in the amygdala, the emotion center of the brain, of people with bipolar when they process emotions like sadness, anger, fear, and joy, and could become a marker to help identify bipolar disorder on brain scans. Likewise, bipolar affects brain biochemistry and neurotransmitters in the brain that produce chemical variations such as oxytocin, GABA, dopamine, and serotonin. These chemicals may be unbalanced in the brains of people with bipolar disorders. But as of yet, researchers aren’t clear on how too little GABA or too many oxytocin-active neurons play a role in the disorder or whether measuring them can help.
Bipolar Disorder in Children and Teens
Bipolar disorders are most common in older adolescents and teens, but children can also be diagnosed with the disorder at a younger age. While not nearly as common in children as it is in adults, research studies have revealed that bipolar disorder affects as many as 3% of all children and up to 7% of children receiving outpatient psychiatric care. (The numbers are even higher in children hospitalized for inpatient psychiatric treatment.) Bipolar disorder has been diagnosed in children as young as 5. When young children experience symptoms, this is called early-onset bipolar disorder.
Bipolar disorder is more likely to affect the children of parents who have the disorder. When one parent has bipolar disorder, the risk to each child is l5 to 30%. When both parents have bipolar disorder, the risk increases to 50 to 75%. (National Institute of Mental Health)
Bipolar in kids also causes distinct mood episodes from mania or hypomania to depression. However, because kids and adolescents can act out, have difficulty in school or at home, and display some of the symptoms of bipolar disorders, like restlessness, impulsivity, risky behaviours, and an inflated view of capabilities, even when they don’t have the disorder, it can be difficult to diagnose.
It is important to note that a number of other childhood disorders cause bipolar-like symptoms, including attention-deficit/hyperactivity disorder (ADHD), oppositional defiant disorder, conduct disorder, anxiety disorders, and major depression. Arriving at the correct diagnosis presents challenges because these and other mental health conditions often occur along with the bipolar disorder.
If your child is struggling with behaviours like a depressed mood, loss of interest in activities, negative thinking, suicidal thoughts, a decreased need for sleep, impulsivity, or aggressive or socially inappropriate behaviour, they should see a mental health professional that specializes in children. And for kids with a family history of bipolar, parents should be vigilant about watching for symptoms and looking for help early. Getting diagnosed and treated earlier can prevent serious consequences and help kids keep their moods in check and manage symptoms from a younger age.
Bipolar Disorder In Women and During Pregnancy
Women and people with bipolar II disorder are significantly more likely to experience periods of rapid cycling than men with the same condition. Other research findings indicate that women with bipolar disorder may have more depressive episodes and more mixed episodes than men with the illness.
Pregnancy and the postpartum period can exacerbate bipolar disorder symptoms. The body goes through so many hormonal changes and women who already have an underlying bipolar disorder can have their symptoms exacerbated by these changes, explains Dr. Narasimhan. Crazy enough, sometimes women who don’t have bipolar disorders can develop one in the postpartum period. Called postpartum bipolar onset, the mood disorder may resolve itself after the postpartum period or it can sometimes remain.
“The general consensus is that when there’s severe mental illness, and someone gets pregnant, it’s not the time to take them off medication,” Dr. Narasimhan says. “That said, you have to have an honest discussion and know which medications have some risk during pregnancy and which can affect the fetus,” she says. Oftentimes the risk of not being on medication is worse than the risk of stopping the medication. Dr. Narasimhan also says she has plenty of patients who don’t want to take their medication during pregnancy, and for these patients, they weigh the risks and benefits carefully.
How is Bipolar Disorder Diagnosed?
There is no simple “test” you can take to determine bipolar disorder. Instead, you’ll need to meet with a provider who specializes in mental health disorders and discuss your specific symptoms.
Your doc will give you a full physical to rule out any underlying medical conditions, such as hyper and hypothyroidism, that could cause manic or depressive states. If none are found, you’ll undergo a series of psychological assessments to gather additional information about your condition and determine which type of bipolar disorder you may be suffering from. Your provider will talk with you to determine your symptoms, their duration, intensity, and frequency, and gauge how your symptoms impair daily life, school, work, and relationships.
Your physician will also consider your family history when diagnosing. If there are family members with bipolar or depression, that’s a red flag for genetic pre-disposition to developing a bipolar disorder, Dr. Narasimhan says. She also asks about any family history of completed suicide or suicide attempts, which is concerning because untreated bipolar disorder can result in suicide. In previous generations, often family members didn’t realize that they had a mental illness or went undiagnosed, misdiagnosed, or never sought treatment. So, when a family has any committed or attempted suicide in their history, it can be a red flag for bipolar.
On the flip side, your family might also play a role in helping you get a diagnosis. Oftentimes, your family, a significant partner, or co-workers are first to recognize signs and symptoms of bipolar disorder. If you’re suffering from this condition, you may be reluctant to seek help at first–mostly because you may not notice how disruptive the disorder is to your life or think it’s just part of your personality. And, you may enjoy feeling high or euphoric when you’re manic.
Whatever your symptoms, we can’t underscore this enough: If you believe you are experiencing signs and symptoms of mania or depression, see your doctor. Bipolar disorder won’t go away on its own, but with the right treatment plan, you can successfully manage it.
How Is Bipolar Disorder Treated?
Medications and psychotherapy are the most commonly prescribed treatment plans for people suffering from bipolar disorder. And the success rate of these plans is very high if you follow them consistently.
Medications
Depending on how severe your symptoms are, your provider may prescribe medication to help get you out of a manic or depressive state. Avoiding drugs and alcohol and taking your medication as prescribed—even on days you feel fine—can help you lead a normal, productive life.
Psychotherapy
Psychotherapy Studies show psychotherapy has also been an effective tool for people living with bipolar disorder. Cognitive behavioral therapy helps you learn how to change negative or harmful thoughts or behaviors.
Family-focused therapies involve family members and focus on teaching you coping strategies, communication, and problem-solving techniques.
Interpersonal and social rhythm therapy (IPSRT) is often used in treating bipolar disorder as well, as this form of psychotherapy focuses on the stabilization of daily rhythms—sleep, wake, mealtimes—to introduce consistent routines to better manage moods.
Dialectical behavior therapy, (DBT) is also an effective treatment for bipolar disorders. DBT concentrates on regulating your emotions better so when you’re manic, you can have tools to help cope, English explains. She says you may do sensory type activities like breath work to calm down or put your feet in water or hold a frozen object to help bring you back to reality and teach you to live in the moment.
Psychoeducation has also been a powerful therapeutic tool to teach those living with bipolar disorder about their condition and how to treat it. This education allows you to notice triggers and impending mood swings so you can seek treatment before a full-blown episode happens.
Other Bipolar Disorder Treatment
Most patients respond very well to medication and various psychotherapies but there are some outliers who don’t respond as well, points out Dr. Narasimhan. In this case, you may want to explore other options.
Transcranial Magnetic Stimulation
Medication-resistant patients can benefit from other treatments such as Transcranial magnetic stimulation (TMS). This non-invasive treatment works by using magnetic fields to stimulate nerve cells in the brain and improve depressive symptoms. The treatment delivers repetitive magnetic pulses via an electromagnetic coil placed against your scalp. Though the mechanism for how it works isn’t well understood, it’s thought to impact how the brain works, which in turn can alleviate depressive episodes. TMS is well tolerated, doesn’t include much downtime, and has only some side effects such as headache, tingling, and lightheadedness. There are some rare side effects such as seizure and hearing loss.
Electroconvulsive Therapy
Electroconvulsive therapy (ECT) involves brief electrical stimulation while the patient is sedated and can be effective for those with severe symptoms that haven’t responded well to medication and psychotherapies. Though, it gets a bad rap thanks to movies and TV from the 40s and 50s, which showed it more like a torture device used on wide-awake patients. But today’s treatment is a lot more civilized and uses electro currents that pass through the brain, which intentionally trigger micro seizures. It’s these micro seizures which may reset the brain’s circuitry and help alleviate symptoms of depression. Though it’s generally safe, side effects can include confusion and memory loss as well physical problems like headache and jaw pain.
Lifestyle and Integrative Treatments
Lifestyle habits such as consistent sleep, regular exercise, a nutritious diet and mindfulness practices such as yoga, meditation have been shown to help improve symptoms of bipolar disorders. Integrative treatments are also something many patients with bipolar disorders may want to explore. Dr. Narasimhan says many, such as organic green tea, have been found to have some efficacy in improving mood symptoms. “There’s some evidence that micronutrient deficiencies, like folic acid or anemia, can be involved, and supplementation may be helpful,” she says. For example, melatonin or magnesium can aid sleep. If you’re interested in exploring integrative treatments for bipolar disorders, talk with your mental health provider, or find an integrative specialist.
Related Mental Health Conditions
These mental health disorders can run in families and may have an overlap with bipolar disorders, meaning researchers have linked genes for these disorders with bipolar. So, if someone in a family has bipolar disorder, it’s common that other family members may have any of the following mental health conditions. A few include:
ADHD, a chronic condition that begins in childhood and can persist into adulthood in which someone has difficulty paying attention, controlling impulses and hyperactivity. Restlessness distracted behavior and constant activity are hallmark signs.
Autism spectrum disorder is a neurological and developmental condition related to brain development that appears early in childhood and impacts how a person perceives and socializes with others, causing problems in their social interactions and communication.
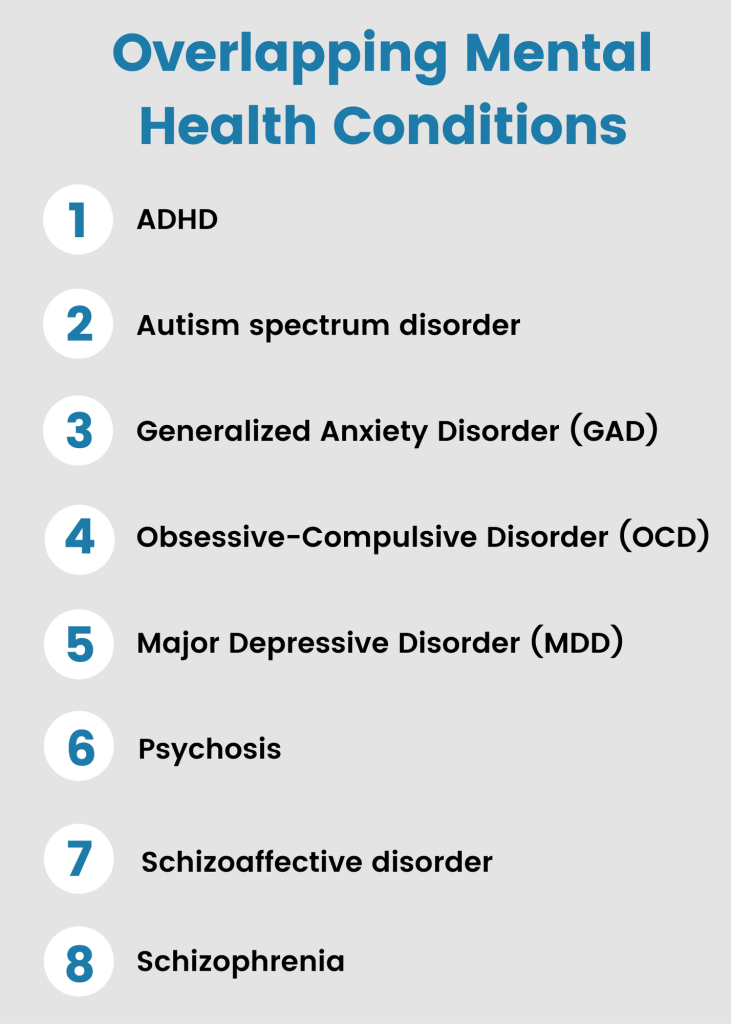
Generalized Anxiety Disorder (GAD) is a mental disorder that’s characterized by excessive and persistent worry and nervous feelings.
Obsessive-Compulsive Disorder (OCD) is an anxiety-based mental health disorder where people have recurring unwanted thoughts and ideas that signal them to act repetitively and compulsively like constant cleaning, handwashing, or checking door locks or appliances.
Major Depressive Disorder (MDD) is a serious mood disorder which causes persistent feelings of sadness and loss of interest in everyday activities. It can interfere with daily life and can include suicidal ideations.
Psychosis is a severe mental disorder or state in which thoughts and emotions are impaired by abnormal thinking and perceptions.
Schizoaffective disorder is a mental health disorder which combines schizophrenia and mood disorders like depression or bipolar. Symptoms like delusions, hallucinations, mania or depressive episodes may occur at the same time or at different times.
Schizophrenia is a serious mental health disorder where people interpret reality abnormally. It’s characterized by hallucinations, delusions, and disordered thinking and behaviours.
Bipolar FAQs
When someone is managing their bipolar disorder well, they likely won’t appear any different from anyone else. If they’re in a manic episode you might notice they talk fast, switch topics continually, have grandiose plans or ideas, or take risks. When in a depressed episode they may have trouble getting out of bed, show a lack of interest in activities they used to love, not engage in conversation, have difficulty socializing or interacting with others, or have suicidal thoughts.
There are times when you feel terrific and productive when you are manic, like you can do anything. But you can also feel out of control with racing thoughts and unable to concentrate long enough to accomplish something. When in a depressed episode, you can feel sad, uninterested in anything, and really low like something terrible must have happened but nothing did.
Both men and women are affected equally and have similar symptoms. However, men usually experience mania first while women typically start with depressive episodes. Women and people with bipolar II disorder are significantly more likely to experience periods of rapid cycling than men with the same condition. Other research findings indicate that women with bipolar disorder may have more depressive episodes and more mixed episodes than do men with the illness.
Absolutely. People with well-managed bipolar disorders have jobs, families, and are productive members of our society. Bipolar disorder, while a chronic condition, doesn’t define you. Just like people who manage their diabetes or heart condition, you can learn to manage and control bipolar disorders with medications, therapies, and good lifestyle habits that sets you up for a successful life.
Bipolar and Suicide
One of the contributors to the decreased life expectancy in BD is suicide. Accordingly, the rate of suicide among BD patients is approximately 10–30 times higher than the corresponding rate in the general population. Extant research found that up to 20% of (mostly untreated) BD subjects end their life by suicide, and 20–60% of them attempt suicide at least one in their lifetime.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6723289/
In addition, bipolar disorder results in 9.2 years reduction in expected life span, and as many as one in five patients with bipolar disorder completes suicide.
Stats from NAMI:
https://www.nami.org/learn-more/mental-health-conditions
1 in 5 U.S. adults experience mental illness each year
1 in 25 U.S. adults experience serious mental illness each year
1 in 6 U.S. youth aged 6-17 experience a mental health disorder each year
50% of all lifetime mental illness begins by age 14, and 75% by age 24
Stats from DBSA:
https://www.dbsalliance.org/education/bipolar-disorder/bipolar-disorder-statistics/
Bipolar disorder affects approximately 5.7 million adult Americans, or about 2.6% of the U.S. population age 18 and older every year. (National Institute of Mental Health)
The median age of onset for bipolar disorder is 25 years (National Institute of Mental Health), although the illness can start in early childhood or as late as the 40’s and 50’s.
An equal number of men and women develop bipolar illness and it is found in all ages, races, ethnic groups and social classes.
More than two-thirds of people with bipolar disorder have at least one close relative with the illness or with unipolar major depression, indicating that the disease has a heritable component. (National Institute of Mental Health)
Prevalence of Bipolar Disorder Among Adults: National Institute of Mental Health. (2019). “Bipolar Disorder.” https://www.nimh.nih.gov/health/statistics/bipolar-disorder.shtml. https://www.cambridge.org/core/journals/psychological-medicine/article/synaptic-and-brainexpressed-gene-sets-relate-to-the-shared-genetic-risk-across-five-psychiatric-disorders/73114566C699FA78AB07B6DE7A6775BC
Family-focused therapy & bipolar disorder: JAMA Psychiatry. (2020). “Affects of Family Focused Therapy vs. Enhanced Usual Care for Symptomatic Youth at High Risk for Bipolar Disorder.” https://jamanetwork.com/journals/jamapsychiatry/article-abstract/2758325
Women and Bipolar. Damone, A. L., Joham, A. E., Loxton, D., Earnest, A., Teede, H. J., & Moran, L. J. (2018). Depression, anxiety, and perceived stress in women with and without PCOS: A community-based study. Psychological Medicine, 49(09))
Bipolar treatment. Current Treatment Options in Psychiatry. (2017). “Treatment of Psychiatric Symptoms Among Offspring of Parents With Bipolar Disorder.” https://link.springer.com/article/10.1007/s40501-017-0126-9
The bipolar brain vs the depressed brain: Biological Psychiatry. (2019). “Amygdala Activation and Connectivity to Emotional Processing Distinguishes Asymptomatic Patients with Bipolar Disorders and Unipolar Depression.” https://www.sciencedirect.com/science/article/abs/pii/S2451902218302362?via%3Dihub
Psycom.net. Bipolar Disorder Signs, Symptoms, and Treatments – Psycom. (2022) [online] Available at: https://www.psycom.net/bipolar-disorder
Women and Bipolar (FAQs) Damone, A. L., Joham, A. E., Loxton, D., Earnest, A., Teede, H. J., & Moran, L. J. (2019). Depression, anxiety and perceived stress in women with and without PCOS: A community-based study. Psychological Medicine, 49(9), 1510-1520. https://doi.org/10.1017/S0033291718002076. Abstract available at: https://research.monash.edu/en/publications/depression-anxiety-and-perceived-stress-in-women-with-and-without
Women and Bipolar (FAQS). Hilty D, Brady K, Hales R. A Review of Bipolar Disorder Among Adults. February 1999. Available at https://ps.psychiatryonline.org/doi/full/10.1176/ps.50.2.201
