Menu
Table of Contents
Depression
Table of Contents
Related Subjects
Tell Me All I Need to Know About Depression
You have questions about depression. Maybe many, many questions: Do I actually have it? What causes it? What treatments are best? We’re going to answer them as clearly and thoughtfully as possible, with help from the top doctors around. Our hope is that you’ll find some peace right now—and plenty of solutions moving forward.
What Is Depression?
Imagine depression as a weather forecast for your mood. There’s a 100% chance of clouds and showers on Monday. Tuesday, too. Wednesday looks just as grim. Actually, the next two weeks show nothing but storms. You’re stuck in this crappy weather pattern and there seems to be no relief in sight.
You might feel alone, but you have lots of company. Depression—or major depressive disorder (MDD), the term for clinical depression—is one of the most common mental health conditions, affecting an estimated 350 million people in all age groups.
And let’s just get this out of the way: Depression isn’t the same as being sad. It’s normal to feel blue or unmotivated from time to time, but depression is more constant. And, it has a real, biological basis. It’s a serious mood disorder that can negatively impact your health and quality of life, as well as those closest to you.
The clinical definition, based on the fifth edition of the Diagnostic and Statistical Manual of Mental Health Disorders (DSM-5), is “a period of at least two weeks when a person experienced a depressed mood or loss of interest or pleasure in daily activities, and had a majority of specified symptoms, such as problems with sleep, eating, energy, concentration, or self-worth.” This definition excludes grief after mourning.
As many as two-thirds of people struggling with depression literally try to grin and bear it—they don’t seek or receive the help they need to cope—and those who do often let months go by before bringing it up with their doctor. Depression can stick around for years if left untreated and can lead to physical symptoms or even thoughts of suicide. Even if an episode resolves on its own, it could recur.
Thankfully, the stigma around mental health conditions like depression continues to lift. And with screening for depression now available within primary care, the hope is that more people gain access to the treatment they need.
How Common Is Depression?
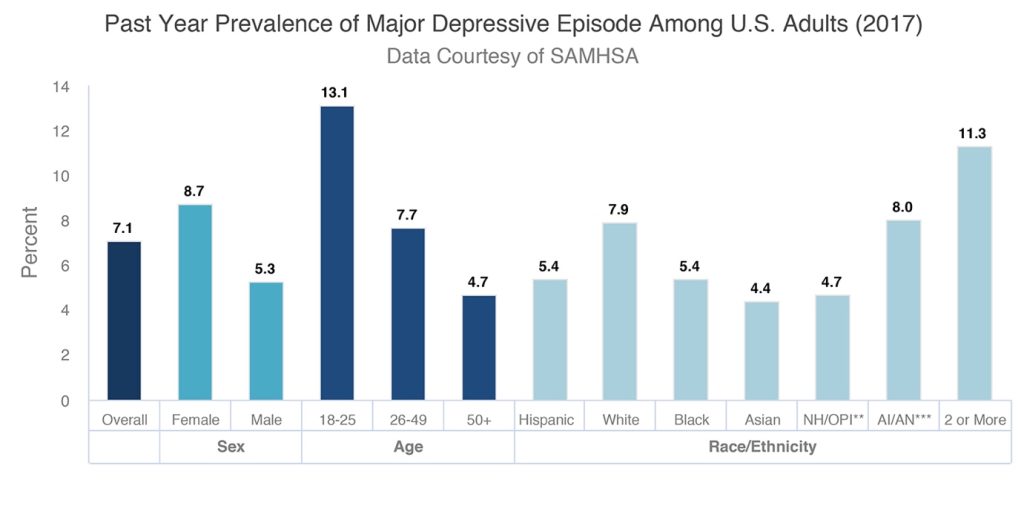
Major depression is one of the most common mental illnesses in the country. An estimated 17.3 million adults in the US reported having at least one major depressive episode over the course of a year, a 2017 report by the Substance Abuse and Mental Health Services Administration (SAMHSA) shows.
That’s 7.1% of all adults ages 18 and older. Women have a higher prevalence of experiencing a major depressive episode than men (8.7% compared to 5.3% for adult males).
Depression is especially crushing for the workforce: It’s the number one leading cause of disability worldwide, according to the World Health Organization. The total economic burden of MDD is estimated to be $210.5 billion per year in the United States alone—a figure that reflects costs associated with missed days, reduced productivity, treatment for depression, and suicide.
What Are the Causes of Depression?
There is no one single cause for the onset of depression because a combination of genetic, biological, environmental, and psychological factors all play a role. These include:
- The brain’s physical structure or chemistry. In some people with depression, brain scans indicate a smaller hippocampus, which plays a role in long-term memory. Research shows that ongoing exposure to stress can impair the growth of nerve cells in this part of the brain.
- Serotonin levels are out of balance. Here’s another thing that’s going on in the brain that may be connected, the serotonin receptors act differently than in someone without depression. This is why some of the treatment drugs work with serotonin.
- History of depression in the family. Someone with a parent or sibling with MDD has a two or three-times greater risk of developing depression than the average person (or a 20-30% chance vs. 10%).
- Genetic code is different. When you’re born you get either a short or a long gene from each parent. These are called alleles. It turns out having one or more short ones is linked to having more of a proclivity towards being depressed when something bad happens.
- History of other disorders or concurrent mental health conditions. Post-traumatic stress, substance use disorders, and learning disabilities are commonly associated with or can perpetuate depression. Anxiety is a big one: Up to 50% of people who have depression also have an anxiety disorder.
- Stressful or major life events. Abuse, financial issues, the death of a loved one, the loss of a job—these situations can all trigger depression. But even positive events like a big move, getting married, graduating, or retiring can make you feel depressed, too. For one these events alter your routine, but they can also trigger feelings that whatever the success or happy occasion is, isn’t deserved.
- Hormone changes. Menstrual cycles, pregnancy, and giving birth can cause bouts of depression.
- Certain physical conditions, like chronic pain or headaches, show a correlation with—or may spur on—depression.
- Certain medications, like sleeping aids and blood pressure medication, may also cause symptoms of depression.
What Are the Different Types of Depression?
Major depression is the classic type of depression and what’s diagnosed, or labeled, as MDD (it’s also known as unipolar depression). People with major depression have symptoms of depression most of the day, nearly every day, for episodes of at least two weeks and can experience recurrent episodes throughout their lives. Under MDD, you can further break down depression into several specific subtypes:
- Seasonal Affective Disorder (SAD) emerges during particular seasons of the year—commonly winter—brought on from diminished natural sunlight.
- Atypical Depression’s biggest differentiator is mood reactivity. People with this kind of depression see their mood improve when something positive happens.
- Bipolar Disorder used to be called manic depression and involves alternating between episodes of depression and extremely elevated energy.
- Psychotic Depression occurs when a person experiences depressive episodes so severe they start having false fixed beliefs (delusions) or hearing or seeing things that others can’t hear or see (hallucinations).
- Postpartum Depression occurs after giving birth. Mothers may feel disconnected from their new baby or fear that they could hurt their child.
- Premenstrual Dysphoric Disorder is a severe type of depression that shows up during the second half of the menstrual cycle.
- Situational Depression, or adjustment disorder, refers to depression that is triggered by a significant life-changing event.
- Persistent Depressive Disorder used to be called dysthymia. It’s a chronic form of depression—usually with milder symptoms—in which an episode lingers for a long period of time, sometimes two years or more. It could be described as feeling like you’re living on autopilot.
Signs and Symptoms of Depression
Experiencing a combination of these symptoms—along with at least a low mood or loss of pleasure—for a period of at least two weeks could signify a depressive episode (for more, see 7 Surprising Symptoms of Depression):
- Persistent feelings of sadness, hopelessness, worthlessness, or emptiness. You generally feel down most of the time.
- Loss of interest in activities—even in stuff you used to love. It’s like you just lose motivation and feel disinterested.
- Trouble sleeping or oversleeping. You have a hard time falling asleep, staying asleep, or getting out of bed. We’re not talking the occasional snooze-hitting; this is like your body is covered in a 50-pound weighted blanket and you can’t get out of bed.
- Appetite or weight changes. You’re overeating, lose your appetite, or experience significant weight gain or loss without dieting (about 20 percent of your weight). Sometimes people get a little rush from eating and so they seek that lift and it leads to over-eating; other times though you may just have no appetite at all.
- Fatigue or decreased energy. You feel exhausted all the time, or you feel like you can spend days on the couch or in bed.
- Difficulty thinking clearly or quickly, remembering details, concentrating, or making decisions. You feel distracted and focusing seems impossible.
- Irritability, frustration, or pessimism. Your mood and headspace feel negative most of the time.
- Physical aches and pains. You may have headaches, stomach-aches, or neck tension.
- Recurrent thoughts of death or suicide, with or without a plan to actually do it. If you or someone else needs help now, contact the Samaritans at 116 123

What Does Depression Look Like?
We’ll raise your question with a few Q’s of our own: Are you female? Are you a teen? Depression can also affect different ages and genders in unique ways:
Women are more likely to ruminate (worry, dwell on, or rehash negative feelings). This can look like negative self-talk, sudden crying spells, feelings of guilt, or blaming oneself. Women are also more likely to have depression at the same time as an anxiety disorder, such as panic disorder, eating disorder, or obsessive-compulsive behavior.
Men with depression are more likely to show signs of irritability, anger, apathy, escapist behavior (like spending more time at work), or reckless behavior (like misusing alcohol or other substances).
Younger people can struggle with depression and MDD (even though the average age of onset is 32). Children and teens may sometimes exhibit oversensitivity, social withdrawal, poor school performance, frequent physical complaints (like headaches and stomachaches), or feelings of incompetence and despair (like they can’t do anything right or that everything is their fault).
Older adults and the elderly are often misdiagnosed or undertreated for depression because their symptoms can be mistaken for other disorders (for example, confusion or memory problems caused by depression can look like Alzheimer’s disease), or they may assume their feelings are just an inevitable part of aging. For many, sadness isn’t the biggest indicator of depression; instead, physical complaints (aches and pains, worsening headaches) are often the predominant symptom. Sleep trouble, low motivation, neglect of personal care or hygiene, and fixation on death are other signs of depression in older adults.
How Is Depression Diagnosed?
These days, a routine doctor’s visit with your general health practitioner may be all it takes to receive a diagnosis. Standard screening tools like the Patient Health Questionnaire (PHQ-9)—a survey of yes, nine items, that physicians use to assess the severity of depression—are becoming widely used in primary care settings to screen for the condition.
In fact, “most patients with depression are going to be diagnosed and treated by primary care doctors, not specialists or psychiatrists,” says James Murrough, M.D., Ph.D., Director of the Depression and Anxiety Center for Discovery and Treatment at Mount Sinai.
Depression is mainly diagnosed by history and clinical presentations, or a specific pattern of symptoms, says Dr. Murrough, which is to say there’s no blood test for MDD. But if you have symptoms like changes in sleep or appetite, your doctor may look into other conditions unrelated to mental health (a thyroid issue is the classic example).
“The first thing your doctor might do is order blood tests—not to make the diagnosis of depression, but to rule out things that could be masquerading as depression,” explains Dr. Murrough. “For example, an underactive thyroid can present as low mood and feeling sluggish, and iron deficiency anemia is another reason why some people might have low energy.”
Ultimately, doctors are looking for a consistent pattern of symptoms that represent a “clear change from the way someone was before, as well as objective signs of functional impairment,” says Dr. Murrough. They’ll ask when your symptoms started and how you felt before, look at your family history, and use your score from the PHQ-9 to aid in the diagnosis. It’s also important to note that when a patient mentions thoughts of suicide, that’s a major red flag.
Depression and Pregnancy
Between hormonal changes, stress, and other environmental changes, getting pregnant can supercharge the D-word.
Perinatal Depression
What to expect when you’re expecting? For as many as 23% of people who conceive, this period can come with the unwelcome arrival of depressive symptoms. Perinatal depression includes major and minor depressive episodes that occur during pregnancy or in the first 12 months after delivery.
During pregnancy, hormone changes can affect the chemicals in your brain, and it can sometimes result in exacerbated anxiety or depression. But possible triggers can also include infertility treatments, previous pregnancy loss, and having complications during pregnancy. The signs and symptoms for depression during pregnancy, also known as antepartum depression, are similar to MDD and can be effectively treated with the right help (even with drug-free approaches like talk therapy).
The Post-Baby Blues
If you experience a bit of emotional “baby blues” after childbirth—mood swings, crying spells, and anxiety that keeps you up at night—go easy on yourself because most new mothers go through this (hello, major life change!). If after two weeks, these symptoms have persisted, it could be postpartum depression.
Studies have shown that one in seven mothers experience postpartum depression in the year after they give birth. People with a previous history of depression may have a higher chance of developing postpartum depression. Talk with your doctor about a game plan for treatment and make it a point to ask for help from friends and family whenever you need it (parenthood is stressful enough!). And as always, remember that perinatal depression is neither shameful, nor a character flaw or sign of weakness.
What Are the Treatments for Depression?
There are ever-evolving ways to treat depression, and the mix will depend on everything from how long you’ve had it and the severity of your symptoms.
Medications
There’s no shame in taking medication to manage your depression. People routinely take medication for physical ailments, and having a mental illness isn’t any different.
Antidepressants work by affecting neurotransmitters in the brain. Common types of antidepressants include selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), and norepinephrine-dopamine reuptake inhibitors (NDRIs). See a list and descriptions of these medications here, and speak with your doctor to determine which drug is right for you. If you’re worried about the possible side effects, remember that any medication can be tapered down or ceased.
One major development that’s under psychopharmacological research for treatment-resistant depression is ketamine, which is used in medicine as an anesthetic. “It’s important to know that ketamine is beneficial for only a very specific subset of the population,” says psychologist Jessica Stern, Ph.D., clinical assistant professor in the Department of Psychiatry at NYU Langone Health, “and is only to be used after several other full courses of therapies—both psychotherapy and multiple other medications—have been tried extensively.” Meaning, ketamine wouldn’t normally be a first or second line of treatment.
Therapy
Who doesn’t go to therapy these days? It’s as much a part of regular conversation as the weather. Psychotherapy (aka talk therapy), sometimes along with medication, can be highly beneficial in treating, managing, and reducing the duration of an episode of depression.
“Evidence-based treatments, such as Cognitive Behavioral Therapy (CBT), Acceptance and Commitment Therapy, and Dialectical Behavior Therapy have been shown to be very effective in the treatment of depression,” says Dr. Stern. “These psychotherapies are active skills-based therapies that help individuals develop and maintain skills to manage difficult thoughts and feelings.”
Trained experts like psychiatrists and psychologists can offer many types of these treatments, from light therapy for seasonal affective disorder to CBT that works to change your thought processes. One goal of CBT includes behavioral activation, an effective treatment and technique in which a therapist can help you schedule more enjoyable activities that bring fulfillment, meaning, or pleasure into your life. According to Dr. Stern, behavioral activation may even potentially decrease the likelihood of depression for those seeing a therapist for reasons other than MDD.
Therapy may be even more accessible now than ever before. Due to the pandemic, over three-quarters of clinicians say they’re now providing their services remotely, primarily via phone or video on a designated telehealth platform. So, you have no excuse not to make an appointment. Whether you have MDD or just everyday mental health struggles, “research has shown, prior to COVID-19 and now increasingly with COVID-19, that telehealth-based psychotherapy is incredibly effective,” Dr. Stern explains. “It allows psychotherapy to be conducted very similarly to in-person psychotherapy, while decreasing barriers that may make it difficult to attend sessions in person.” In other words, there’s no need to travel or find childcare, and your session happens comfortably in your own home.
Other Treatments
“Device treatments such as Transcranial Magnetic Stimulation (TMS) and Electroconvulsive Therapy (ECT) may be beneficial and appropriate for certain individuals,” adds Dr. Stern. TMS, ECT, and vagus nerve stimulation (VNS)—a newer treatment that involves surgically implanting a device similar to a pacemaker along the peripheral nerve in the neck—are all types of brain-stimulating approaches that may sound very sci-fi but can be effective after first trying therapy and medication.
Healthy Habits
Any treatment for depression should coincide with maintaining a healthy diet, regular exercise, a productive sleep schedule, and—yes—even mindful self-care practices. These are all helpful in alleviating or reducing the severity of symptoms, says Dr. Stern.
Exercise helps you better cope with stress, and the endorphins released during exercise may give you a mental boost. Increased research shows that “exercise and physical activity can have significant effects on depression, and particularly in those with mild-to-moderate depression,” she adds. “This may include cardiovascular workouts, stretching, or mindfulness-based physical activity like yoga.” The Centers for Disease Control and Prevention (CDC) reports that physical activity also helps you sleep better at night—setting off a chain reaction for a more supportive routine.
Meditation is another highly effective way of clearing your head and calming your body. You can also try keeping a journal—some people find that it helps to express their thoughts on paper instead of bottling them inside. Talk to close friends and family about your struggles, too. Having a social support system plays a key part in maintaining your mental health and wellbeing.
Recovery is a journey, not a destination. Bad days will still come, but with well-targeted treatment, you should be able to overcome extreme lows. While science has yet to find a cure for mental disorders such as depression, it is entirely possible to live a happy and fulfilling life in spite of it.
Relationship RX
The catch-22 with depression is that your social network is incredibly important for maneuvering through feeling better, but it’s so easy to sabotage your connections to friends and family because you think you want to be alone, or you become so withdrawn that people start to leave you alone. Read our article, “Living with a Depressed Person” if someone you care about is in a bad place.
Depression and Suicide Risk
Depression usually does not lead to suicide ideation. But, according to the US Department of Health and Human Services, studies have shown that about two percent of people who have been treated for depression in an outpatient setting will die by suicide. If the treatment is inpatient, the number doubles to four percent. Men are more likely to die by suicide after depression than women. Find hotlines and organizations for support in our emergency mental health resources directory.
Depression FAQs
There is no single cause of depression, but there are factors that might increase the chance of it. Theses include death or loss, abuse, other traumatic events, certain medications, genetics, substance abuse, and more.
Depression is most likely to occur in adults between the ages of 45 and 65.
Helping someone with depression might not look a single way. However things that you can do to help include encouraging treatment, listening with compassion, helping the person suffering with daily tasks, be vigilant for signs of sucidal behaviour, and to make sure you are caring for yourself, too.
China has the highest rates of unipolar depressive disorders in the world.
Surprisingly, some experts say that it can. “For some people, depression is cyclical or seasonal, and they can eventually recover and remit without any specific intervention,” says James Murrough, M.D., Ph.D., Director of the Depression and Anxiety Center for Discovery and Treatment at Mount Sinai. “But we also know that treatments like psychotherapy and medications can severely reduce the symptoms and duration of an episode of depression. Many individuals who suffer from depression never seek treatment, and that’s why from a public health perspective we want to keep reducing the stigma around it.”
“While there’s no surefire way to prevent depression, one of the greatest protective factors for depression is social connection and social support,” says Jessica Stern, Ph.D., clinical assistant professor in the Department of Psychiatry at NYU Langone Health. Maintaining healthy friendships and relationships, she says, “can potentially significantly decrease the likelihood or severity of depression.” What’s more, the chance that an individual will receive care for symptoms of depression is often based on their social situation, Dr. Murrough says. “Friends or family notice that someone’s not themselves, having trouble getting out of bed, and missing activities and appointments, and will help them seek care.” Someone who’s relatively isolated may be at risk for not getting treatment, and in turn, fall into deeper depression. The key? Nurture your relationships and encourage each other to talk openly about your feelings, without judgment. The more we can de-stigmatize emotions, the more we can help “prevent or slow down the progression of negative emotions to depressive symptoms,” says Dr. Stern.
Those most at risk for developing depression include women, the elderly, those with a personal or family history of depression, chronic stressors, those with other concurrent mental and physical health conditions, low socioeconomic status, and those taking medications that may cause depression, like birth control or some anxiety medications.
When you experience a loss of someone close to you, it’s normal to grieve and feel down and empty for a period of several weeks or more, “but it should get better,” says Dr. Murrough. “If you’re starting to feel worse instead of better as time goes on, that’s a red flag.” Perhaps, more critically, a typical grief reaction isn’t: “My life is not worth living anymore.” Consider seeking treatment if you or someone experiences this.
While no specific diet has been proven to relieve depression, a healthy diet can help you feel your best physically and mentally. Certain foods may be linked to brain health and support for memory, alertness, and mood. Examples include foods that contain omega-3 fatty acids (found in nuts and fatty fish like salmon), antioxidants (blueberries, broccoli), and nutrients like choline (found in egg yolk). Always talk with your doctor before making any major diet changes.
Helpful Resources If You’re Depressed
Depression hotlines can help—right now. If you are experiencing a mental health crisis, or if someone you love is in danger, reach out to a qualified mental health professional.
Here are some quick numbers for free, confidential support 24/7 if you need help now:
For emergencies:
Call 999
For suicide prevention:
116 123
Estimated figures on worldwide prevalence of depression and disability: World Health Organization. (2012). Depression: A Global Public Health Concern.
The total economic burden of MDD. Journal of Clinical Psychiatry. (2015). The economic burden of adults with major depressive disorder in the United States (2005 and 2010).
Prevalence of perinatal depression. American College of Obstetricians and Gynecologists. 2015. Screening for Perinatal Depression.
Prevalence of postpartum depression. JAMA Psychiatry. 2013. Onset Timing, Thoughts of Self-harm, and Diagnoses in Postpartum Women With Screen-Positive Depression Findings.
Current trends in telehealth. American Psychological Association. 2020. Psychologists embrace telehealth to prevent the spread of COVID-19.
Soriano, K. – Psycom.net. (2022). Depression Types, Causes, Symptoms, Statistics, & Treatment. [online] Available at: https://www.psycom.net/depression
