Menu
Table of Contents
PTSD
Table of Contents
Related Subjects
Post-Traumatic Stress Disorder (PTSD): Understanding PTSD Symptoms and Causes
If you have experienced a terrifying traumatic event and now suffer from post-traumatic stress disorder as a result, treatment does exist, and following it can help you to rebuild your life. To get the most of your treatment plans, follow these pieces of advice:
• Learn all you can about your disorder and what effects it has on your body – this allows you to recognize signs and symptoms and coping strategies
• Follow the treatment plans prescribed to you by your doctors and mental health providers – even if you are feeling “fine”
• Don’t turn to drugs and alcohol to “numb” your feelings
• Stay healthy – eat well-balanced meals and exercise on a regular basis
• Find support groups that can help you through difficult times – and to have a support base that you can talk to about anything
Post-Traumatic Stress Disorder, or PTSD, is a mental health disorder that may develop after experiencing or witnessing a scary or life-threatening event. Learn more about the causes, symptoms, and effective treatment options here.
What Is PTSD?
If you live through a terrifying event or experience, such as a horrific car crash, a killer tornado that cripples your hometown, or domestic violence, you are likely to feel shattered and experience difficulty coping and adjusting. However, as time goes on, and with good individual care, you are likely to be able to cope with this post-traumatic stress and move on with your life.
On the other hand, if you can’t stop reliving the experiences and it affects your everyday functioning, you might be suffering from post-traumatic stress disorder (PTSD).
One of the few mental illnesses triggered by an outside, traumatizing event, you can suffer from PTSD by experiencing or witnessing a terrifying event.
What is considered traumatic? Certain traumatic events can be so severely frightening and overwhelming to individuals that they can cause temporary and sometimes permanent changes to how we physically and psychologically respond to stress in our lives. You may find yourself wondering what types of trauma can cause these changes to our physical and psychological responses. Any unexpected violation to our physical and mental well-being can be considered a trauma.
Some of the most common traumatic events that may lead to post-traumatic stress disorder include:
- The sudden death of a loved one
- Critical illness and near-death experience, and subsequent stay in the Intensive Care Unit (ICU). In a 2015 Johns Hopkins study, researchers found that nearly 25% of ICU survivors suffer from PTSD.
- War
- Rape
- Kidnapping
- Natural disasters (e.g., tornadoes, earthquakes, hurricanes)
- Terrorist attacks
- Car or plane crashes
- Assault
- Sexual or physical abuse
- Childhood neglect
Similarly, a person witnessing a traumatic event happening to a loved one (such as their child, parent, or significant other) may also experience PTSD.
Not everyone who experiences a traumatic event will suffer from PTSD. As mentioned above, it’s normal to have nightmares, be fearful, and find difficulty “forgetting” what happened. When you get stuck in a state of fear and shock and your symptoms don’t improve or get worse, post-traumatic stress disorder is likely settling in because your body is having problems restoring itself to equilibrium.
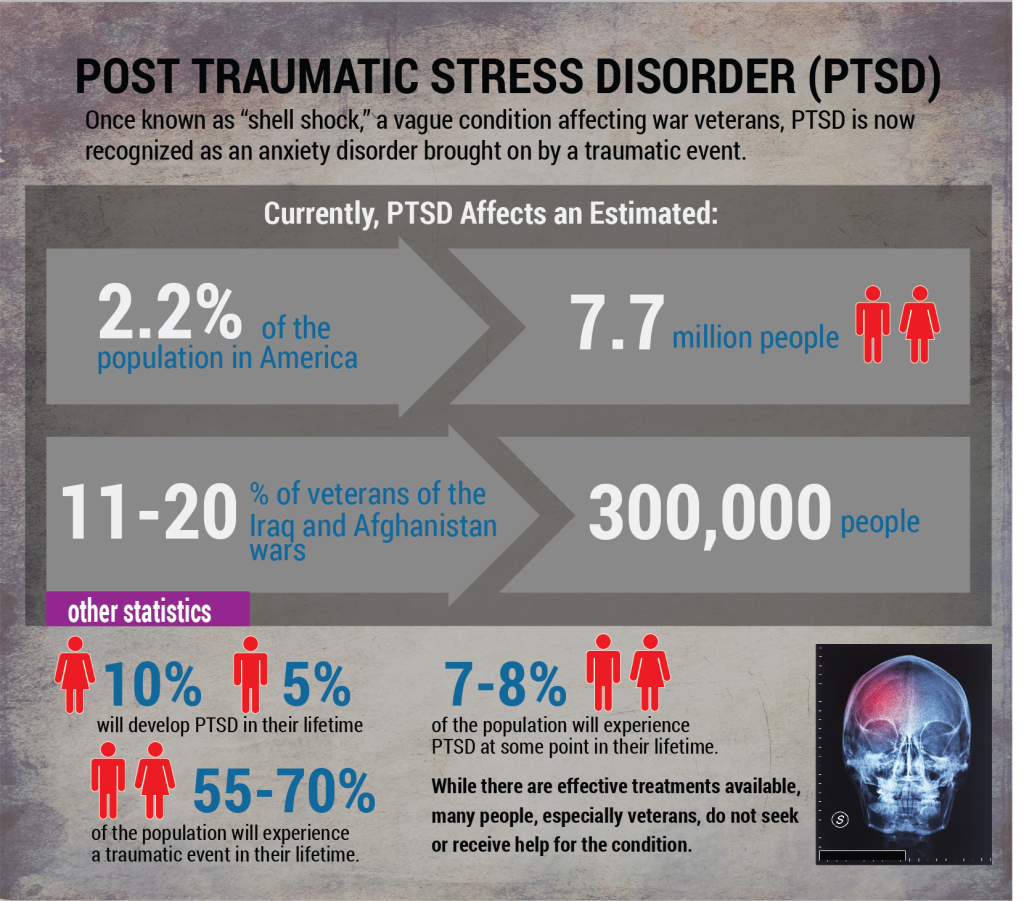
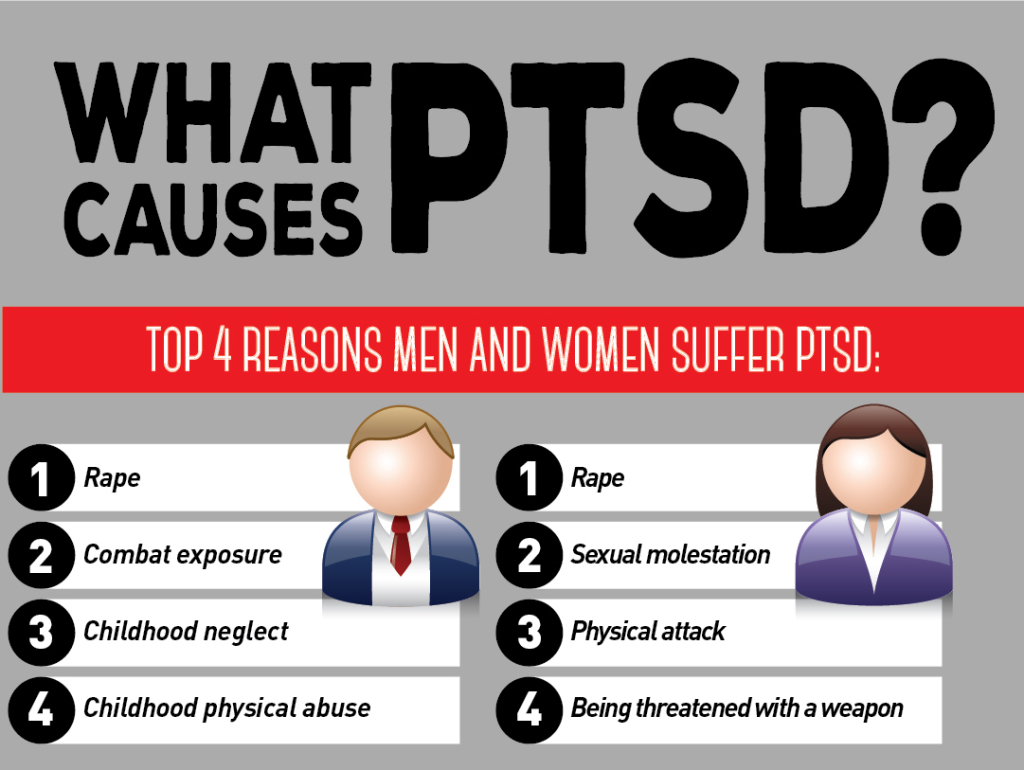
PTSD is found to occur in approximately 1 in 10 individuals affected by a traumatic event. On average, 60% of men and 50% of women experience a traumatic event during their lifetimes. Of these, 4% of men are found to develop PTSD and 10% of women are found to develop PTSD at some point in their lives. Individuals experiencing rape have a higher likelihood of developing post-traumatic stress disorder over any of traumatic event; therefore, as women are more likely to be raped than men (9% vs. 1% likelihood), this explains the imbalance in the statistics of post-traumatic stress disorder among genders.
Additional research shows the majority of individuals affected by post-traumatic stress disorder also suffer from another psychological disorder (e.g., depression, anxiety). These individuals are also more prone to problems with substance abuse of drugs and/or alcohol.
PTSD Symptoms
There is no way of knowing who will develop post-traumatic stress disorder after a traumatizing event. As evidenced by past research, the majority of people who witness or live through a traumatic event will not suffer from PTSD. Most will likely have memories of the events, but their lives will not become negatively impacted by it in their daily interactions.
Symptoms of PTSD are often grouped into types. These types include: avoidance, intrusive memories, changes in emotional reactions, and negative changes in thinking and mood. The most common symptoms of post-traumatic stress disorder include flashbacks, jumpiness (literally “jumping out of one’s skin”), emotional detachment. These symptoms can come and go and vary in intensity. We outline the four types below:
Avoidance Symptoms
- Avoiding talking about or thinking about the traumatic event
- Avoiding places, activities, or people that remind you of the traumatic event
Intrusive Memories
- Flashbacks – reliving the event as if it were happening all over again
- Upsetting dreams/nightmares about the traumatic event
- Recurrent memories of the traumatic event – even when you are trying not to think about them – as if they won’t “leave your mind”
- Experiencing severe emotional distress or physical reactions to things that remind you of the traumatic event
Changes in Emotional Reactions
- Overwhelming guilt or shame
- Jumpiness – being easily startled or frightened – jumping out of your skin
- Sleep disturbances
- Difficulty concentrating
- Always in “defense” mode – on guard for danger
- Irritability
- Angry outburst
- Aggressive behavior
- Self-destructive behavior (e.g., reckless driving, substance abuse)
Negative Changes in Thinking and Mood
- Feeling negatively about yourself and others
- Lack of interest in activities you once found enjoyment in
- Difficulty maintaining relationships with others
- Memory problems – not being able to remember parts of the traumatic event
- Feelings of hopelessness for the future (e.g., marriage, career, living a normal life span)
- Emotional numbness – feeling detached from others
- Inability to experience positive emotions
PTSD Symptoms in Children
Children and adolescents may exhibit slightly different symptoms of post-traumatic stress disorder than adults. These symptoms include:
- Severe separation anxiety – fear of being separated from their parents
- Somber play that showcases a revival of the traumatic events
- Phobias unrelated to the traumatic event (e.g., fear of monsters)
- Acting out the traumatic experience through drawings, social play, or stories
- Loss of previously acquired skills (e.g., regression in toilet training, reversion in motor skills, changes in communication skills such as starting to stutter or stammer when speaking, and, most commonly, becoming selectively mute)
- Sleep problems and nightmares not related to the event
- Irritability and aggression
- Aches and pains that have no apparent cause
PTSD Causes, Risk Factors, and Diagnosis
You are more likely to suffer from post-traumatic stress disorder if the traumatic event you endure is life-threatening or severely traumatic to your personal safety. Additionally, the more exposure to the event or prolonged exposure to a traumatic event is also more likely to increase your chances of developing PTSD. Other risk factors of post-traumatic stress disorder include:
- Family history of PTSD and depression
- History of physical or sexual abuse
- High level of stress in your daily life
- Lack of coping skills
- Not getting help or support after the traumatic event
- History of depression, anxiety, or other mental illness
- History of substance abuse
- Careers that exposure you to traumatic experiences (e.g., military, police, first responders)
- Experiencing previous traumatic events, especially early in one’s life
- The extent that the traumatic event was uncontrollable, inescapable, or unexpected
- Type of traumatic event – intentional, human-afflicted harm (e.g., rape, sexual abuse) is more likely to result in PTSD than an act of God (e.g., hurricane, earthquake) or self-destructing behavior (e.g. drinking excessively to the point of organ damage, a car accident caused by drunken driving resulting in permanent bodily damage, or smoking excessively, leading to health issues such as lung cancer)
Suffering from post-traumatic stress disorder can increase your chances for other mental illnesses, such as depression and anxiety, suicide, eating disorders, and issues with drugs and alcohol. Therefore, it is especially important to seek treatment if you are suffering from PTSD for your own well-being. You should seek treatment for post-traumatic stress disorder if you are experiencing any of these symptoms and are not able to function or cannot function effectively in your day-to-day life.
Individuals may be affected differently by the symptoms of PTSD. PTSD symptoms in women, men, and children may present themselves in a variety of situations depending upon the trauma they have experienced.
Diagnosis of post-traumatic stress disorder is completed by medical professionals. Your diagnosis will be based on psychological evaluations of your signs and symptoms. To be diagnosed with post-traumatic stress disorder, you must meet the criteria listed in the Diagnostic and Statistical Manual of Mental Disorders published by the American Psychological Association. In addition to experiencing or witnessing a traumatic event, you must experience one or more of the following after exposure to the traumatic event:
- Reliving the traumatic event
- Upsetting dreams/nightmares about the traumatic event
- Experience of flashbacks
- Experience of emotional distress related to the traumatic event
In combination with these symptoms, you may also experience debilitating behaviors and emotions one month or more post-traumatic event to include things such as avoidance behaviors, memory loss, emotional numbness, self-destructive behavior, and difficulty sleeping.
Your doctor or mental health professional will then make a diagnosis of post-traumatic stress disorder and refer to you a number of treatment options.
PTSD Treatment
Several types of treatment options are available if you are suffering from post-traumatic stress disorder. The most often prescribed method of treatment is psychotherapy. Medications and other types of physical treatment options are also prescribed. Your doctor will formulate the best treatment course of action for you.
Psychotherapy, often referred to as “talk therapy” has been shown to elicit great responses from sufferers of post-traumatic stress disorder. Cognitive therapy is focused on recognizing patterns of thinking that get you “stuck” in your emotional state. For example, this type of therapy might help you in recognizing cognitive patterns associated with negative perceptions of normal situations.
Exposure therapy is often coupled with cognitive therapy if you have been diagnosed with PTSD. Exposure therapy focuses on safe exposure to what is causing you intense fear. This exposure enables you to cope with the stimulus effectively and rationally. Eye movement desensitization and reprocessing (EMDR) is a form of therapy that combines exposure therapy with guided eye movements. The combination of guided eye movements and exposure therapy helps you in your cognitive processing of traumatic events and allows you to effectively change your reactions to these types of events.
PTSD Medications
Medication can be useful in treating post-traumatic stress disorder. Two types of medication have been found to be especially beneficial: antidepressants and anti-anxiety medications.
Selective serotonin reuptake inhibitors (SSRIs), including Zoloft and Paxil, have been approved by the Food and Drug Administration as antidepressant treatments for PTSD.
Anti-anxiety medications are typically prescribed short-term to relieve severe anxiety problems associated with PTSD. They are usually only prescribed temporarily because of the ease of addiction to this type of medication.
Nightmare suppressant drugs (i.e. Prazosin) may also be prescribed if you are suffering from post-traumatic stress disorder to help you sleep more easily and with fewer disruptions.
What You Can Do Right Now
If you have experienced a terrifying traumatic event and now suffer from post-traumatic stress disorder as a result, treatment does exist, and following it can help you to rebuild your life. To get the most of your treatment plans, follow these pieces of advice:
- Learn all you can about your disorder and what effects it has on your body – this allows you to recognize signs and symptoms and coping strategies
- Follow the treatment plans prescribed to you by your doctors and mental health providers – even if you are feeling “fine”
- Don’t turn to drugs and alcohol to “numb” your feelings
- Stay healthy – eat well-balanced meals and exercise on a regular basis
- Find support groups that can help you through difficult times – and to have a support base that you can talk to about anything
PTSD FAQs
Written by Farah Fazel, PsyS, a licensed clinical, psychometric and school psychologist
There are several symptoms associated with Post-Traumatic Stress Disorder, not just 17. PTSD symptoms are generally grouped into four types: Intrusive Memories, Avoidance Behaviors, Negative Changes in Thinking & Mood, and Changes in Physical & Emotional Reactions.
Individuals with PTSD may experience any of the symptoms under each of the following groups:
- Intrusive Memories:
• Recurrent, unwanted distressing memories of the traumatic event
• Re-living the traumatic event as if it were happening again (flashbacks)
• Upsetting dreams, night terrors or nightmares about the traumatic event
• Severe emotional distress or physical reactions to something that reminds them of the traumatic event - Avoidance Behaviors:
• Trying to avoid thinking or talking about the traumatic event
• Avoiding places, activities or people (triggers) that remind them of the traumatic event - Negative Changes in Thinking & Mood:
• Negative thoughts about oneself, other people or the world
• Hopelessness about the future
• Memory problems, including not remembering important aspects of the traumatic event
• Difficulty maintaining close relationships
• Feeling detached from family and friends
• Lack of interest in activities they once enjoyed
• Difficulty experiencing positive emotions
• Feeling emotionally numb - Changes in Physical and Emotional Reactions (also called Arousal Symptoms):
• Being easily startled or frightened
• Always being on guard for danger
• Self-destructive behavior, such as drinking too much or driving too fast
• Trouble with normal sleep pattern
• Trouble concentrating
• Irritability, moodiness, angry outbursts, or aggressive behavior
• Overwhelming guilt or shame
In general, the most common physical and behavioral symptoms of PTSD include:
- Vivid flashbacks and re-living the event; triggers lead to disturbing memories of the traumatic event, as if they are happening all over again and causing intense emotional and physical reactions.
• Disturbances in sleep pattern; the ability to fall asleep and stay asleep requires humans to let their guards down. Disruption in sleep normalcy can include hypersomnia (over-sleeping), hyposomnia (under-sleeping), intransitive sleep (not being able to stay asleep during sleep cycle), and insomnia (difficulty falling sleep).
• Difficulty with focus and concentrating throughout the day. It is also common that once the person is able to focus on tasks, their attention starts to wander.
• Mood swings and emotion dysregulation; the person starts having positive and negative thoughts simultaneously. One minute, the person can feel positive, thinking they survived the trauma, and another minute they feel the agonizing experience they went through. The shift in thoughts causes daily escalation in mood.
• Emotional eating; in order to distract the brain from painful thoughts, the brain focuses on the pleasant sensation of comforting foods.
• Night terrors, nightmares and disturbing dreams.
• Blocking out the trauma-based event; this is the brain’s coping mechanism where the cortexes that are strongly associated with stress “store” the traumatic event out of surface.
• Low self-esteem and feeling negatively about oneself; low self-worth and not seeing the good in the world, other people or oneself.
• Disassociation and avoiding the cause of trauma. For example, if a person faced the traumatic event in a car crash, they may avoid getting in a car. Or, if a person was attacked by someone in public, that may result in agoraphobia and avoiding going to public places or, in severe cases, having extreme and irrational fear of leaving their home altogether.
• Social avoidance and becoming distant and disengaged from friends, family and loved ones.
Complex Post-Traumatic Stress Disorder (C-PTSD) is a psychological disorder that can develop in response to exposure to an extremely traumatic series of events in a context in which the individual perceives little or no chance of escape, and particularly where the exposure is prolonged or repetitive. Individuals with C-PTSD experience emotional dysregulation; negative self-beliefs; feelings of shame, guilt or failure regarding the trauma; and interpersonal difficulties.
C-PTSD relates to the trauma model of mental disorders and is associated with chronic situations involving captivity or entrapment. The symptoms of C-PTSD can include prolonged feelings of terror, worthlessness, and helplessness, and deformation of one’s identity and sense of self that takes years to overcome and/or will never go away.
Provide support, but accept that you need to give them space. Don’t pressure someone with PTSD into talking, because it can be very difficult for them to talk about their traumatic experience.
Comfort for someone with PTSD comes from feelings of engagement and acceptance, not talking. So instead, let them know you’re there for them to listen when or if they want to talk. Comfort and support can help overcome feelings of helplessness and despair, and it is an important factor in PTSD recovery.
Be patient; recovery is a process that takes time and often involves setbacks. The important thing is to stay positive and maintain support. Accept (and expect) mixed feelings.
Be an active listener; while you shouldn’t push a person with PTSD to talk, if they do choose to share, try to listen without expectations or judgments. Make it clear that you’re interested and that you care, but don’t worry about giving advice.
A person with PTSD may need to talk about the traumatic event over and over again. This is part of the healing process, so avoid the temptation to tell your loved one to stop rehashing the past and move on. Instead, offer to talk as many times as they need. It is very important to respect their feelings and reactions. If you come across as disapproving, horrified, or judgmental, they are unlikely to open up to you again.
When talking to an individual with PTSD make sure you don’t:
• Stop them from talking about their feelings or fears.
• Offer unsolicited advice or tell them what they “should” do.
• Invalidate, minimize, or deny their traumatic experience.
• Tell them they were lucky it wasn’t worse.
• Take over with your own personal experiences or feelings.
Rebuild safety: Trauma alters the way a person sees the world, making it seem like a perpetually dangerous and frightening place. It also damages people’s ability to trust others and themselves. If there’s any way you can rebuild their sense of security, it will contribute to their recovery.
You can rebuild their sense of safety and trust by:
- Expressing your commitment and that you’re here for the long haul, so they feel loved and supported.
• Creating routines. Structure and predictable schedules can restore a sense of stability and security to people with PTSD. Creating routines could involve getting them to help with simple tasks or simply “being there” for the person.
• Minimizing stress. Try to make sure they have space and time for rest and relaxing.
• Speaking of the future and making plans. This can help counteract the common feeling among people with PTSD that their future is limited.
• Keeping your promises. Help rebuild trust by showing that you’re trustworthy. Be consistent and follow through on what you say you’re going to do.
• Emphasizing their strengths. Tell them you believe they’re capable of recovery, and point out all of their positive qualities and successes.
• Looking for ways to empower them. Rather than doing things for them that they’re capable of doing for themselves, it’s better to build their confidence and self-trust by giving them more choices and control.
There are many ways to deal with PTSD: joining a PTSD support group, practicing relaxation techniques, confiding in a person you trust, spending time with positive people who uplift you, listening to soothing music and meditating, and motivating yourself to get back to routine. If your symptoms don’t improve over time and are preventing you from enjoying life, seek help from a mental health professional.
Post-traumatic stress disorder symptoms may start within one month of a traumatic event, but sometimes symptoms may not appear until years after the event. These symptoms cause significant problems in social or work situations and in relationships. They can also interfere with your ability to go about your normal daily tasks. Symptoms can vary over time or vary from person to person.
If you have experienced a trauma or if you have witnessed a loved one experiencing trauma and are finding it difficult to return to normalcy, enjoy life or participate in activities that you once enjoyed, then you may have PTSD.
Generally speaking, PTSD feels like reoccurring panic attacks and often involves having vivid flashbacks of the traumatic event and having intense and disturbing thoughts related to the shocking experience. The emotional impact can surface as fear, anger, shame, guilt, low self-esteem, and negative outlook on life. The traumatized person can feel the need to detach or estrange themselves from other people, and they may have mood swings, experience sleep disturbances, or avoid triggers that remind them of the traumatizing experience.
Gregory C. – Psycom.net – What is PTSD? Post-Traumatic Stress Disorder Symptoms and Causes. (2022) [online] Available at: https://www.psycom.net/post-traumatic-stress-disorder/ [Accessed 15 May 2022].
